Stride Stronger: Physiotherapy for Diabetic Neuropathy
Physiotherapy Post | Vol. 3, Issue 84 | July 2025
Dear Readers,
Welcome to this insightful edition of Physiotherapy Post, titled “Stride Stronger: Physiotherapy for Diabetic Neuropathy.” In a world where diabetes continues to rise at an alarming rate, one of its most challenging complications—diabetic neuropathy—remains a significant barrier to independence, mobility, and quality of life.
In this issue, we delve into the critical role of physiotherapy in restoring function, alleviating pain, and improving gait patterns in individuals affected by peripheral nerve damage due to diabetes. From targeted balance training and foot care education to neuromuscular re-education and proprioceptive strategies, physiotherapy stands as a pillar of holistic diabetic care.
Let us walk you through the latest research, therapeutic exercises, and evidence-based interventions that help patients not just walk—but stride stronger toward a better tomorrow.
Stay informed. Stay empowered.
Warm regards,
Dr. Aditi Singh
Editor-in-Chief, Physiotherapy Post
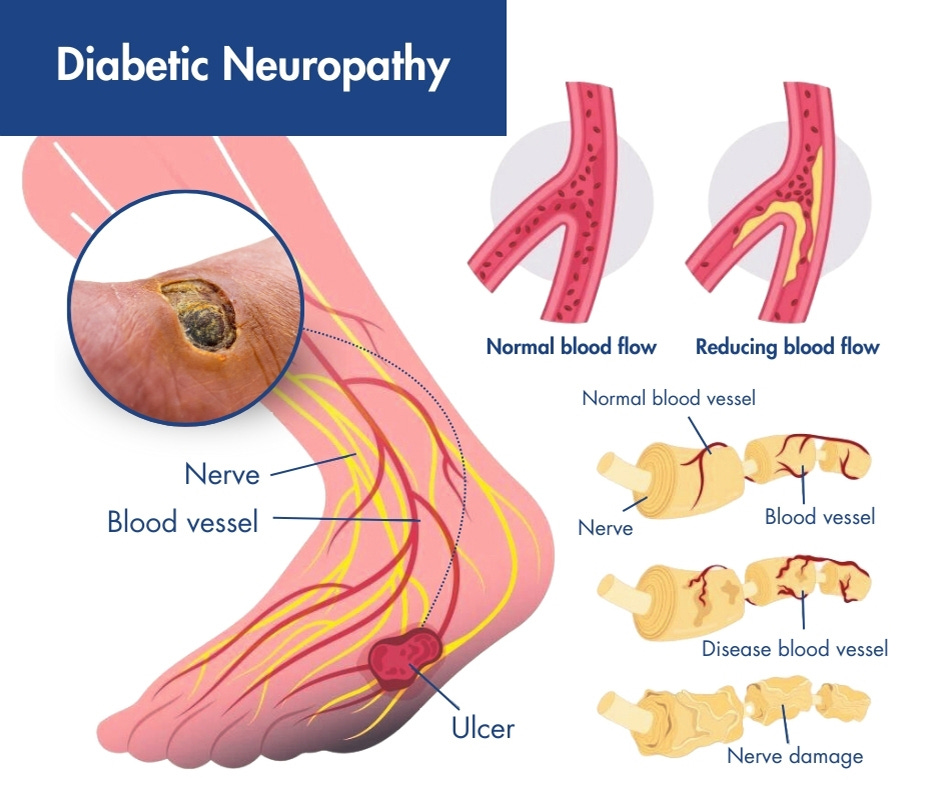
Diabetic peripheral neuropathy (DPN) is the most prevalent form of diabetic neuropathy, characterized by a progressive loss of nerve fibers, especially in the distal lower extremities. Symptoms range from pain, burning, and paraesthesia to profound sensory loss and motor weakness. This leads to impaired balance, altered gait mechanics, muscle atrophy, and increased risk of foot ulcers and falls.
Central Role of Physiotherapy
Physiotherapists contribute to the multi-disciplinary management of DPN by targeting four key areas:
Neuromuscular Reconditioning
Postural and Gait Restoration
Fall Prevention and Balance
Foot Health and Ulcer Prevention
Key Evidence-Based Physiotherapy Interventions
1. Progressive Balance Training
Evidence: A randomized controlled trial by Allet et al. (2010, Diabetes Care) showed that DPN patients participating in an 8-week structured balance and coordination program had:
28% improvement in Berg Balance Scale scores.
Significant reductions in postural sway (both eyes-open and eyes-closed conditions).
Decreased fear of falling (FES-I scores).
Interventions:
Static/dynamic balance drills (e.g., single-leg stance, Bosu ball training).
Dual-task training for cognitive-motor coordination.
Sensory enhancement (e.g., barefoot walking on textured surfaces).
2. Gait Retraining & Functional Mobility Enhancement
Findings from Cavanagh et al. (2012, Gait & Posture): Individuals with DPN demonstrate:
Reduced ankle power generation.
Increased step width and double stance time.
Therapy Approaches:
Treadmill walking with visual/auditory feedback.
Functional task training: sit-to-stand, stair negotiation, and community ambulation.
Video-based gait analysis and correction.
3. Strength Training for Lower Limb Musculature
Evidence: Mueller et al. (2008, Physical Therapy Journal) reported that resistance training in DPN patients:
Improved ankle dorsiflexion and plantarflexion strength.
Increased 6-minute walk distance.
Protocols:
Closed kinetic chain exercises (mini squats, step-ups).
TheraBand resistance programs.
Intrinsic foot muscle strengthening (toe curls, marble pickups).
4. Sensory Re-education and Tactile Stimulation
Rationale: Sensory loss leads to foot deformities and ulcers.
Methods:
Vibration therapy to improve proprioception.
Mirror therapy and graded sensory exposure.
Education on self-checks, foot inspection, and footwear modification.
5. Neuromuscular Electrical Stimulation (NMES)
Evidence: A meta-analysis (Chen et al., 2021, Journal of Rehabilitation Research) confirmed that NMES significantly:
Enhances lower limb muscle strength.
Promotes nerve reinnervation.
Reduces pain and improves daily function.
Target Groups:
Elderly DPN patients with muscle atrophy.
Individuals with poor volitional contraction.
6. Assistive Devices and Orthotic Management
Clinical Insight: DPN patients often benefit from orthotic support to redistribute plantar pressures and stabilize gait.
Strategies:
Use of ankle-foot orthoses (AFOs) for foot drop.
Customized insoles for offloading pressure points.
Training in the use of canes or walkers to enhance safety.
Preventive Physiotherapy: A Step Ahead
Regular physiotherapy monitoring helps delay the progression of DPN.
Patient education is crucial for early recognition of symptoms, foot hygiene, and ulcer prevention.
Clinical Pearls for Practitioners:
Screen for sensory loss using 10g monofilament or vibration tests.
Prioritize early referral to physiotherapy even in asymptomatic patients with diabetes.
Incorporate motivational interviewing to improve long-term adherence to home exercise programs.
News update:
1. 5 ‘Toxic’ Foods a Heart Expert Would Never Give Kids And What They Eat Instead
Read more at: Link
When Looking Young Becomes an Obsession: The Psychological Toll of Anti-Ageing Pressure
Read more at: Link
Early onset of cardiac issues a pointer to lifestyle changes, lack of physical activity: Ravindranath
Read more at: Link
NEW COURSES from Welcome to SmartCARE Education!
Online Certified Dry Needling Professional
Online Certified Dry Needling Professional for chiropractors and physical therapists. Master Dry Needling from the comfort of your own home. Get credentialed, improve your patient outcomes and increase your revenue.
Dry Needling in Chiropractic for Orthopedic and Sports Conditions-
Optimizing Training and Injury Prevention Across the Menstrual Cycle in Female Athletes
Upcoming event/s:
Thought of the Week:
Have questions or need personalized guidance?
Our expert team is here to help! Feel free to reach out at editorphysiotherapypost@gmail.com — we’d love to hear from you.
Wishing you strength, vitality, and pain-free days ahead.
Warm regards,
Team Physiotherapy Post